A process perspective answers key questions in an iterative and systematic way to guide a set of complex needs through to validated and effective operational systems.
Contents
Introduction
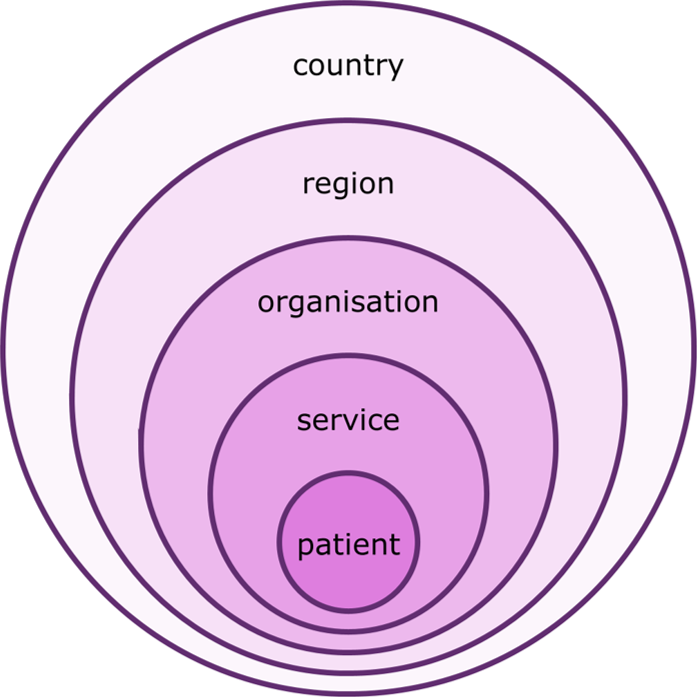
The successful management of improvement in complex systems is a practical challenge requiring an understanding of people, systems, design and risk perspectives along with improvement management skills. In this context, the questions associated with these perspectives have been rationalised where they overlap and improvement programme questions have been added. The have then been reordered to provide a natural sequence for all the questions. The resulting Systems Approach can be applied to the design and improvement of systems at all extremes of scale, with service level improvement taking place at a local level or within a wider context that may subsequently require changes at the organisation level and cross-organisational level.
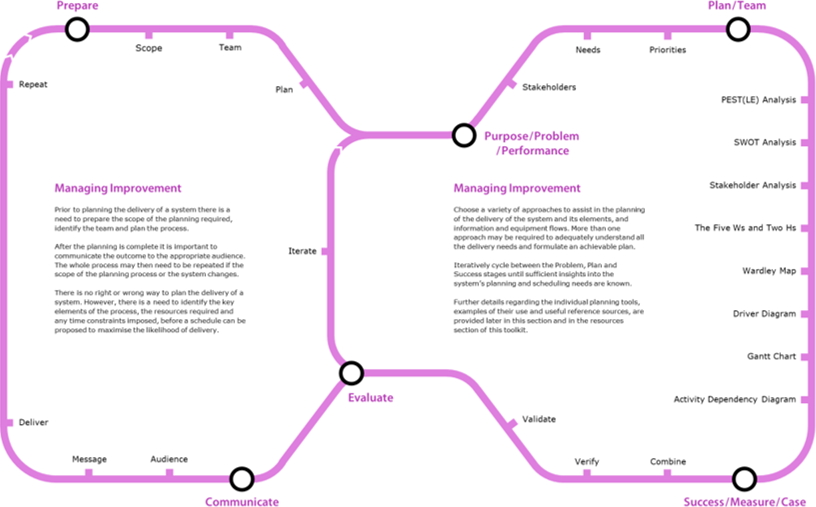
It is useful to consider the process of improvement to be made up of a series of iterative purpose / problem / performance, plan / team and success / measure / case cycles that enable progress from understanding what is known about the system through to developing successful interventions to the system. This are preceded by a trigger and supported by the formation and ongoing management of a team. The current and better questions are assumed to be incorporated in the organise and explore questions described later in this section of this toolkit. Active management is appropriate at all stages of a product or service lifecycle, from early conception, through use to disposal.
Questions
Trigger
Why are we doing this?
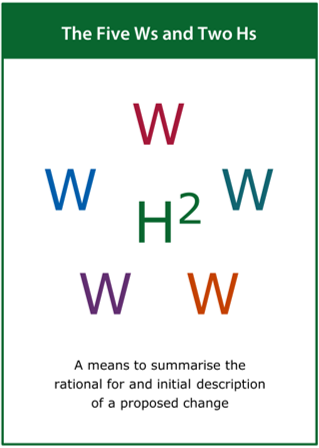
The trigger phase asks the question ‘Why are we doing this?’ and leads to a documented rationale for improving an existing system or developing a new one, with regard to the timing, source and particular nature of the trigger. It is likely to include a variety of activities that can help capture this rationale, for example:
- Record the trigger for the improvement process
- Identify the initial scope of the improvement process
- Ensure that an appropriate team is assembled
All improvement processes are initiated, and potentially shaped, by their trigger1, which may classed as:
- Strategic — where risk reduction and improvement is part of an ongoing strategic initiative.
- Incident — where an event has resulted in actual or potential harm to patients or clinicians.
- Local — where the potential for incidents has been identified locally.
- Routine — where a team or individual wishes to check the integrity of their service.
- Improvement — where changes are planned to an existing service or system.
- New — where a new service is to be introduced into practice or an existing one decommissioned.
- Technology — where new equipment or technology is to be introduced to an existing service.
- Estates — where estates or buildings are being built, refurbished or maintained.
- Staff — where new staff are to be introduced to an existing service or exiting staff levels are changed.
- External — where specific strategic changes or checks are externally requested.
- National — where teams are encouraged to propose and deliver national service improvements.
A clear understanding of the trigger helps to identify the initial scope of the improvement and ensures that an appropriate team is assembled to initiate any subsequent improvement process. Whether the trigger relates to people, systems, design or risk, a systems approach should consider all of these perspectives in a seamless and integrated way.
Footnotes
- Engineering Better Care, a systems approach to health and care design and continuous improvement. Royal Academy of Engineering, London, UK, 2017.
Purpose
What is the purpose?
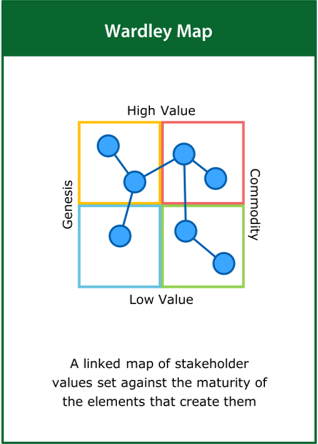
The purpose phase asks the question ‘What is the purpose?’ and leads to detailed description of the purpose of the current system within its wider context, based on an understanding of the system and the behaviour and level of performance it is expected to deliver. It is likely to include a variety of activities that can help develop this description, for example:
- Provide a detailed description of the purpose of the system
- Understand the wider context of care and therefore of the system
- Identify factors that influence the performance of the system
Current
What do we do now?
The current phase asks the question ‘What do we do now?’ and leads to a detailed description of the current system architecture and its observable behaviour based on observation, active enquiry and analysis of available information. It is likely to include a variety of activities that can help develop this description, for example:
- Provide a detailed description of the current system
- Understand the operation and behaviour of key pathways
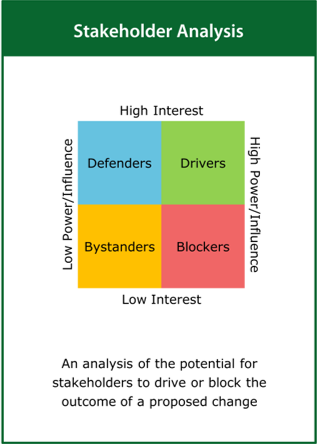
- Identify stakeholders and users and their current needs
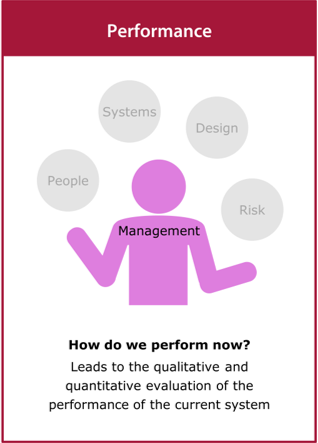
Performance
How do we perform now?
The performance phase asks the question ‘How do we perform now?’ and leads the qualitative and quantitative evaluation of the performance of the current system, with particular regard to the key elements of the system and their expected behaviour. It is likely to include a variety of activities that can help build this understanding, for example:
- Analyse available quantitative data relating to the current system
- Gather qualitative information relating to the current system
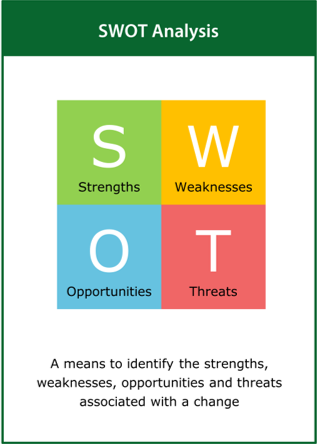
- Identify strengths and weaknesses of the current performance
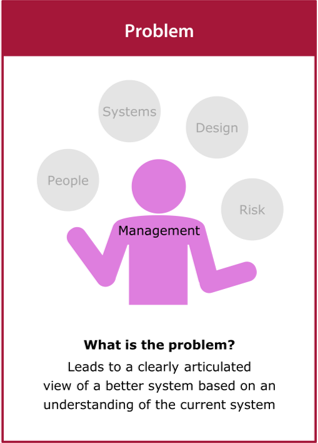
Problem
What is the problem?
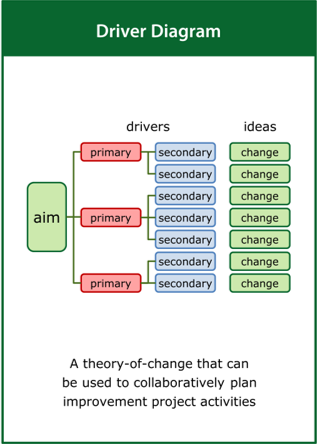
The problem phase asks the question ‘What is the problem?’ and leads to a clearly articulated view of a better system based on an understanding of the current system and the level of improvement desired to achieve acceptable system performance. It is likely to include a variety of activities that can help build this view, for example:
- Describe the current system and its performance
- Describe a future system and its potential performance
- Define the challenge based on the desired improvement
Success
What does ‘good’ look like?
The success phase asks the question ‘What does ‘good’ look like?’ and leads to a common and clearly articulated understanding of success and how it might be recognised, with particular regard to reasonable constraints on its delivery. It is likely to include a variety of activities that can help build this understanding, for example:
- Dream of an ideal goal where there are no constraints
- Define a feasible goal reflecting reasonable constraints
- Create a balanced and viable case for change
Better
How could we improve?
The better phase asks the question ‘How could we improve?’ and leads to a preliminary description of a better system architecture and its intended behaviour, with regard to the current system architecture and its behaviour. It is likely to include a variety of activities that can help develop this description, for example:
- Provide a preliminary description of a future improved system
- Describe the operation and behaviour of key pathways
- Identify stakeholders and users and their future needs
Measure
What should we measure?
The measure phase asks the question ‘What should we measure?’ and leads to the identification of possible performance indicators for the improved system, with regard to the proposed system architecture and its intended behaviour. It is likely to include a variety of activities that can help with this identification, for example:
- Describe the intended performance of the improved system
- Identify possible performance indicators for the improved system
- Outline approaches to measure the agreed performance indicators
Team
Who should be involved?
The team phase asks the question ‘Who should be involved?’ and leads to a common and clearly articulated understanding of who should deliver the improved system, with regard to the differing needs at different stages of the delivery. It is likely to include a variety of activities that can help build this understanding, for example:
- Choose a team that reflects the key stakeholders
- Include members who are active in the current system
- Include members who are able to facilitate change
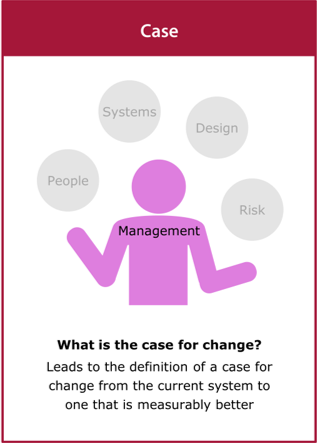
Case
What is the case for change?
The case phase asks the question ‘What is the case for change?’ and leads to the definition of a case for change from the current system to one that is measurably better, with regard to the proposed system architecture and its intended behaviour. It is likely to include a variety of activities that can help with the development of the case for change, for example:
- Compare the current performance to that which is measurably better
- Estimate the value of the proposed system improvement
- Offset the likely value of the change against the cost of change
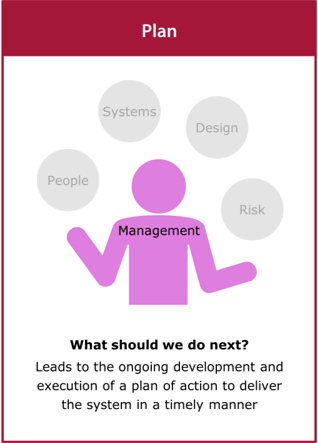
Plan
What should we do next?
The plan phase asks the question ‘What should we do next?’ and leads to the ongoing development and execution of a plan of action to deliver the system in a timely manner, with regard to the resources available for its delivery. It is likely to include a variety of activities that can help with this development, for example:
- Identify the next steps critical to achieving progress
- Build in iteration and contingency to allow for potential problems
- View the plan as a starting point rather than a fixed schedule
Process
Useful toolkit resources: the Process worksheet and cards for each of the tools can be downloaded from the Resources part of this toolkit.
Tools
Literature
British Standards (2008). BS ISO 7000-1:2008 Design management systems — guide to managing innovation. British Standards, London, UK.
Davidoff F, Dixon-Woods M, Leviton L and Michie S (2015). Demystifying theory and its use in improvement. BMJ Quality and Safety, bmjqs-2014-003627.
Dixon-Woods M & Martin G (2016) Does quality improvement improve quality? Future Hospital Journal, 3(3):191-194.
Fillingham D, Jones B, Pereira P (2016), The challenge and potential of whole system flow. The Health Foundation, London UK.
Ham C, Berwick D and Dixon J (2016). Improving quality in the English NHS: a strategy for action. King’s Fund, London, UK.
Langley GL, Moen R, Nolan KM, Nolan TW, Norman CL, Provost LP (2009). The Improvement Guide: A Practical Approach to Enhancing Organizational Performance (2nd edition). San Francisco: Jossey-Bass Publishers.
McGuire KJ and Spear SJ (2015). Beyond the Jargon: architecture, process and clinical care, Spine, 40(16):1243-1246.
Snowden DJ, Boone ME (2007). A Leader’s Framework for Decision Making. Harvard Business Review, BR0711.
The Health Foundation (2013). Quality improvement made simple: what everyone should know about health care quality improvement. The Health Foundation, London, UK.
Feedback
We would welcome your feedback on this page:
Privacy policy. If your feedback comments warrant follow-up communication, we will send you an email using the details you have provided. Feedback comments are anonymized and then stored on our file server
Read more about how we use your personal data. Any e-mails that are sent or received are stored on our mail server for up to 24 months.